| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 4, Number 1, March 2015, pages 191-192
Atraumatic Subdural Hematoma in Preeclampsia With Lethal Outcome
Orivaldo Alves Barbosaa, d, Jose Walter Correiaa, Paola Lima Lemosb, Elson Jose de Almeida, Juniorc, Antonio Eliezer Arrais Mota Filhoc, Isabela Pires Vitoriano de limac
aInternal Medicine Service, Hospital Cesar Cals, Brazil
bNeurology, Hospital Cesar Cals, Brazil
cObstetrics Clinic, Hospital Cesar Cals, Brazil
dCorresponding Author: Orivaldo Alves Barbosa, Hospital Cesar Cals, Emperor Avenue, 545, Centro, Fortaleza, Ceara, Brazil
Manuscript accepted for publication February 17, 2015
Short title: Atraumatic Subdural Hematoma
doi: http://dx.doi.org/10.14740/jcgo311w
| Abstract | ▴Top |
Preeclampsia occurs in about 8% of pregnancies, causing significant morbidity and mortality in this patient population. Subdural hematoma atraumatic absence of coagulopathy is a rare complication of preeclampsia. We present a case of a 31-year-old female with 33 weeks of gestation, who sought treatment for high blood pressure, headache, and proteinuria. After cesarean delivery, the patient developed headache thunderclap and papilledema, and a computed tomography scan revealed a subdural hematoma in the left parietal region, with edema and midline deviation. The patient developed cardiac arrest probably due to herniation. The article reviews the neurological complications of pregnancy and delivery, focusing on subdural hematoma.
Keywords: Subdural hematoma; Pregnancy; Preeclampsia
| Introduction | ▴Top |
Preeclampsia is a multisystem disease characterized by the beginning of new hypertension (systolic blood pressure > 140 mm Hg and/or DBP > 90 mm Hg) and proteinuria (> 0.3 g in 24 h or protein relations/creatinine urine > 0.3) in the second half of pregnancy happening in around 5-7% of pregnancies [1].
Mortality of pregnancy hypertension disease occurs primarily by hypertensive emergency (acute pulmonary edema and aortic dissection), liver failure and cerebrovascular complications [2]. Intracranial bleeding disorders are rare and have high mortality, being more common secondary to intracerebral hemorrhage of the rupture of the aneurysm and arteriovenous malformations [3, 4]. The spontaneous subdural hematoma is extremely rare in this context, having poor prognosis, and requiring immediate diagnosis and treatment [1]. We report a case of a young patient with subdural hematoma in the postpartum period, evolving to lethal outcome.
| Case Report | ▴Top |
This study was approved by the Research Ethics Committee of the Hospital Cesar Cals, Fortaleza, Ceara. The patient’s relatives agreed with the report, according to CNS 196/96.
A 31-year-old female patient with a history of prior cesarean delivery for preeclampsia was admitted to the HGCC with gestational age of 33 weeks and 3 days and headache frame holocranial, intensity 4/10, with no irradiation, associated with blurred vision, the increase in blood pressure (150 × 100 mm Hg), 24-h proteinuria 3.528 mg and lower limb edema. Obstetric ultrasound showed single pregnancy, longitudinal, cephalic, with fetal weight 2,297 g, ILA 84 mm, previous body placenta and Doppler of fetal-placental circulation and normal middle cerebral artery. Corticosteroids were prescribed and magnesium sulfate was opted for pregnancy resolution, being held cesarean delivery without complications under spinal anesthesia. On the third postoperative day, the mothers of newborns developed occipital headache of moderate intensity, no improvement or worsening with recumbency or standing position, in thunder, intensity 10/10 associated with photophobia, phonophobia and vomiting. The examination of eye showed papilledema and diffuse hyperreflexes.
CT scan showed subdural hematoma in the left region, with edema and midline deviation to the contralateral side (Fig. 1). The patient had laboratory tests normal, including dosage of platelets and coagulation tests. Neuroprotection and analgesia measures were initiated, and the patient was moved to state the reference neurosurgery service. Unfortunately, about 48 h after diagnosis, she developed cardiac arrest not reversed, for alleged brain herniation, evolving to death.
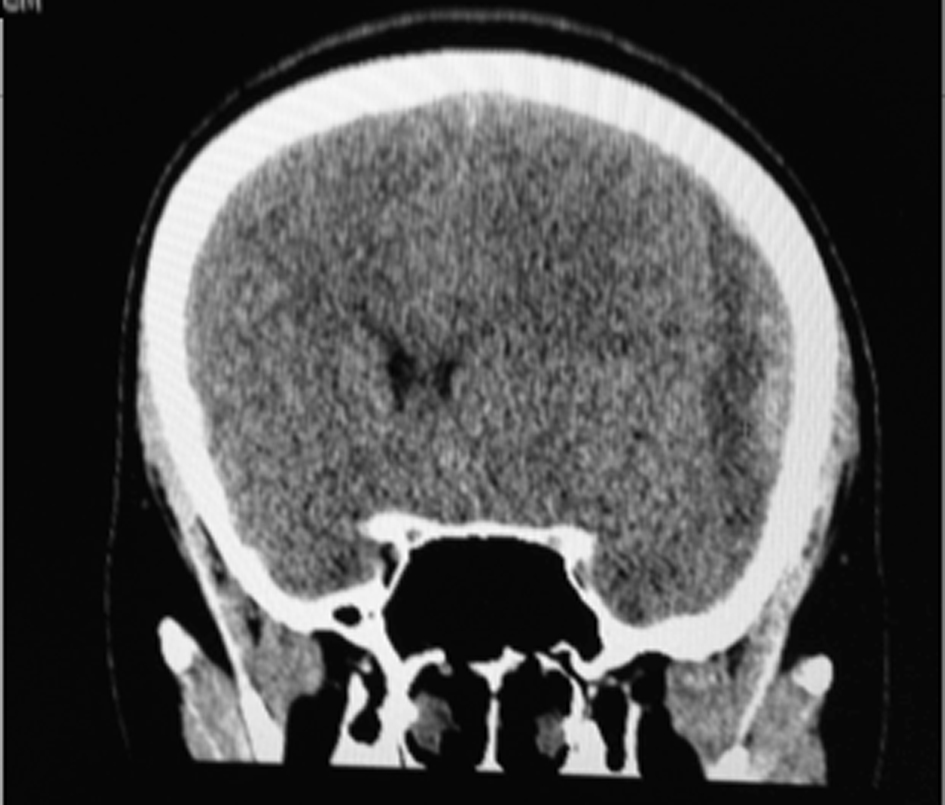 Click for large image | Figure 1. Skull CT showing acute subdural hematoma in fronto-temporo-parietal region, with midline deviation. |
| Discussion | ▴Top |
Subdural hematoma is a common condition, complicating around 1% of head trauma, and refers to the presence of blood in the virtual space between the dura and arachnoid. Most cases occur after trauma, coagulopathy, dural metastases, meningiomas and aneurysms, and are extremely rare in the context of pregnancy and postpartum.
The hypertensive specific disease of pregnancy (HDP) can be understood as a diffuse endothelial pathology, being at the heart of its pathophysiology increasing protein as the Fms-like tyrosine kinase, a factor that blocks angiogenesis, responsible for placental hypoperfusion and systemic dysfunction [5]. Neurological disorders in pregnancy and postpartum are relatively common and can be classified into three categories [6]: 1) do not related to pregnancy status (e.g. intracranial neoplasms); 2) previous neurological disorders (e.g. multiple sclerosis); 3) diseases whose incidence increases during pregnancy.
The case reported is included in the third category. The brain-vascular disease has a higher incidence in pregnancy for several reasons, among them, fluid overload, which can result in hypertension, high levels of estrogen with known prothrombotic effect and endotheliopatia related to preeclampsia [1]. The most frequent pathologies in this context are the posterior reversible encephalopathy, reversible cerebral vasoconstriction of the syndrome and ischemic stroke. Rarely, intracranial bleeding in such patients is usually related to previous aneurysms, arteriovenous malformations of the rupture and bleeding disorders (thrombotic thrombocytopenic purpura, HELLP syndrome, and disseminated intravascular coagulation). Regarding subdural hematomas not traumatic in pregnancy and the postpartum period, there are few reports in the literature, and are most associated with HELLP syndrome [4], with concomitant parenchymal bleeding. Little is known about the pathophysiology of these cases [6], with some reports of subdural hematomas after obstetric anesthesia in patients without preeclampsia [7, 8].
In our case, probably the hypertension associated with endotheliopatia’s own HDP and spinal anesthesia caused the pathophysiological basis for the occurrence of subdural hematoma.
Conclusion
Subdural hematomas, although rare in the context of gestational hypertension, should be considered in the differential diagnosis of headache in pregnancy and puerperium, especially when there is a focal neurological sign and/or thrombotic microangiopathy. In our case, the patient did not have thrombocytopenia, coagulopathy or other risk factors for intracranial hemorrhage, having evolved with lethal outcome, allegedly by brain herniation secondary to intracranial hypertension syndrome.
Conflicts of Interest
The authors do not have conflicts of interest.
| References | ▴Top |
- Duley L, Meher S, Abalos E. Management of pre-eclampsia. BMJ. 2006;332(7539):463-468.
doi pubmed - Sharshar T, Lamy C, Mas JL. Incidence and causes of strokes associated with pregnancy and puerperium. A study in public hospitals of Ile de France. Stroke in Pregnancy Study Group. Stroke. 1995;26(6):930-936.
doi pubmed - Bateman BT, Schumacher HC, Bushnell CD, Pile-Spellman J, Simpson LL, Sacco RL, Berman MF. Intracerebral hemorrhage in pregnancy: frequency, risk factors, and outcome. Neurology. 2006;67(3):424-429.
doi pubmed - Yokota H, Miyamoto K, Yokoyama K, Noguchi H, Uyama K, Oku M. Spontaneous acute subdural haematoma and intracerebral haemorrhage in patient with HELLP syndrome: case report. Acta Neurochir (Wien). 2009;151(12):1689-1692.
doi pubmed - Steven K. Feske, Stroke in Pregnancy. Semin Neurology. 2007;27(5):442-452.
doi pubmed - Edlow JA, Caplan LR, O'Brien K, Tibbles CD. Diagnosis of acute neurological emergencies in pregnant and post-partum women. Lancet Neurol. 2013;12(2):175-185.
doi - Thons M, Neveling D, Hatzmann W. [Intracerebral subdural hematoma after delivery with peridural catheter anesthesia]. Z Geburtshilfe Perinatol. 1993;197(5):235-237.
pubmed - Garcia-Sanchez MJ, Prieto-Cuellar M, Sanchez-Carrion JM, Galdo-Abadin JR, Martin-Linares JM, Horcajadas-Almansa A. [Chronic subdural hematoma secondary to an accidental dural puncture during lumbar epidural anesthesia]. Rev Esp Anestesiol Reanim. 1996;43(9):327-329.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.