| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Original Article
Volume 3, Number 3, September 2014, pages 93-96
Duration of the Development of Twin-Twin Transfusion Syndrome
Shunji Suzuki
Department of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, 5-11-12 Tateishi, Katsushika-ku, Tokyo 124-0012, Japan
Manuscript accepted for publication August 11, 2014
Short title: Development of TTTS
doi: https://doi.org/10.14740/jcgo270w
| Abstract | ▴Top |
Background: It is generally recommended that monochorionic diamniotic (MD) twin pregnancies be followed by ultrasound examination at least every 2 weeks in order to be able to promptly diagnose twin-twin transfusion syndrome (TTTS). In this study, we retrospectively investigated the clinical significance of TTTS developing at < 2 weeks (n = 9) and ≥ 2 weeks (n = 13).
Methods: We examined the following potential factors associated with TTTS development: discordance of the crown-rump length at 8 - 11 weeks, the gestational age at the last confirmation of concordant amniotic fluid (AF), the gestational age at TTTS diagnosis, the estimated fetal weight discordance, and AF values at ≤ 3 - 7 days before TTTS diagnosis.
Results: There were no significant differences in these variables between the two groups.
Conclusion: There were no significant differences in the clinical histories of TTTS developing at < 2 weeks and ≥ 2 weeks in MD twin pregnancy.
Keywords: Twin-twin transfusion syndrome; Duration of development; Amniotic fluid discordance; Concordant amniotic fluid
| Introduction | ▴Top |
Twin-twin transfusion syndrome (TTTS), which is defined as the presence of hydramnios in one sac and oligohydramnios/anhydramnios in the other sac, occurs at a frequency of 8-15% in monochorionic diamniotic (MD) twin pregnancies [1-6]. TTTS is the result of unbalanced blood flow through placental anastomoses between the twins. Left untreated, mortality and morbidity rates due to TTTS have been reported to approach 80-100% [1-6]. The severity of TTTS is classically staged using the Quintero staging system [7]. Intervention at an earlier Quintero stage may lead to better pregnancy outcomes. It is generally recommended that MD twin pregnancies be followed by ultrasound examination at least every 2 weeks in order to be able to diagnose TTTS at an earlier Quintero stage [1-3, 7]. However, when TTTS is diagnosed during the management of MD twin pregnancies by ultrasound examination every 2 weeks, it has sometimes already become serious. Therefore, an additional factor for the prediction of TTTS developing within 2 weeks may be needed.
In this study, therefore, we retrospectively investigated the clinical significance of TTTS developing at < 2 weeks and ≥ 2 weeks in MD twin pregnancies.
| Methods | ▴Top |
We reviewed the obstetric records of 22 cases of MD twin pregnancies complicated by TTTS in which we could observe the process of TTTS developing with an ultrasound examination interval of 3 - 7 days. All cases received prenatal care before 12 weeks’ gestation at Japanese Red Cross Katsushika Maternity Hospital between 2004 and 2013. TTTS was recognized with the presentation of an oligohydramnios-polyhydramnios sequence in MD twin pregnancies, i.e., the largest vertical amniotic fluid (AF) pocket in the donor sac < 2 cm and > 8 cm in the recipient sac [7, 8]. The stage of TTTS was defined using the Quintero staging system [7]. In this study, when the largest vertical AF pocket of both fetuses was between 3 and 7 cm and the difference in the largest vertical AF pocket was ≤ 3 cm, we recognized the finding as “concordant AF” [9]. During the study period, in our institute, MD twin pregnancies with concordant AF and normal fetal growth were usually managed with an ultrasound examination interval of 1 - 2 weeks. If concordant AF or normal fetal growth could not be confirmed in MD twin pregnancies, management with an ultrasound examination at 3 - 7 days intervals was performed.
In this study, potential factors associated with TTTS development were selected according to previous studies: maternal age, parity, the value of discordance of crown-rump length (CRL) at 8 - 11 weeks’ gestation, the gestational age at the last confirmation of concordant AF, the gestational age at TTTS diagnosis, the estimated fetal weight discordance, the AF values at ≤ 3 - 7 days before TTTS diagnosis, and the Quintero staging at TTTS diagnosis [1-5, 10-12]. Discordances in intertwine CRL and the fetal weight were calculated between the two fetuses, and expressed as a percentage of the larger measurement.
Cases (TTTS developing at < 2 weeks) and controls (TTTS developing at ≥ 2 weeks) were compared by Student’s t-test for continuous variables, and the Chi-square or Fisher’s exact test for categorical variables. Differences with P < 0.05 were considered significant.
| Results | ▴Top |
During the study period, there were 436 MD twin pregnancies. Of these, there were 35 cases (8.0%) diagnosed with TTTS, and we could observe the process of TTTS developing with an ultrasound examination interval of 3 - 7 days in 22 cases of them. (During this study period, there were 13 cases of TTTS referred to our hospital because of being deemed high risk based on obstetric consultation at other clinics or hospitals.) Of the 22 cases of TTTS, the developmental durations of TTTS were < 2 weeks in nine cases (41%; average duration: 1.5 ± 0.3 weeks), and ≥ 2 weeks in 13 cases (59%; average duration: 4.3 ± 3.4 weeks). There were no significant differences in the average maternal age or parity between the two groups of TTTS developing at < 2 and ≥ 2 weeks (P = 0.62 and 0.61, respectively).
Table 1 shows a summary of the patients in the two groups with TTTS developing at < 2 and ≥ 2 weeks. There were no significant differences in these variables between them. The rate of early Quintero staging (≤ stage II) in the group with TTTS developing at < 2 weeks did not differ from that of the ≥ 2 weeks group (67% vs. 69%, respectively, P = 0.73). In addition, there were no significant differences in the discordance of CRL at 8 - 11 weeks’ gestation (7.6 ± 3.6 vs. 5.5 ± 4.6%, respectively, P = 0.25) or fetal weight in the period of the last concordant AF between the groups with TTTS developing at < 2 and ≥ 2 weeks (11.0 ± 6.7 vs. 8.9 ± 5.4%, respectively, P = 0.45).
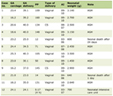 Click to view | Table 1. Summary of Patients With Twin-Twin Transfusion Syndrome Developing at < 2 and ≥ 2 Weeks |
At 3 - 7 days before TTTS diagnosis, oligohydramnios and polyhydramnios were observed in three (33%) and three (33%) patients in the group with TTTS developing at < 2 weeks, while they were observed in three (23%, P = 0.68) and four (31%, P = 0.86), respectively in the ≥ 2 weeks group.
| Discussion | ▴Top |
The main objective of the management strategy for MD twin pregnancies is to detect TTTS in its early stages, thereby allowing for the effective counseling of patients, more timely intervention, and better outcomes [1-5, 13]. Although it is accepted that MD twin pregnancies should be managed by ultrasound examination at least every 2 weeks in order to be able to diagnose TTTS at an earlier Quintero stage, little is known about the natural history of TTTS, such as the progression of the disease.
In this study, there were no significant differences in the clinical significance of TTTS developing at < 2 weeks and ≥ 2 weeks in MD twin pregnancy, excluding the duration of development. Although some useful observations have been reported to predict the development of severe TTTS, we could not identify an additional factor for the prediction of TTTS developing within 2 weeks. Previous studies advocated moderately discordant AF in the (early) second trimester as a predictor of the subsequent development of TTTS. However, in this study, there were no significant differences in AF between TTTS developing at < 2 weeks and ≥ 2 weeks.
In this study, the average gestational age at the time of confirming the last concordant AF in the group with TTTS developing at < 2 weeks was 22.6 ± 6.5 weeks, compared to 17.8 ± 4.1 weeks in the ≥ 2 weeks group. The difference did not reach significance (P = 0.06). The gestational age may not affect factors determining TTTS development; however, there is a possibility of the association between the timing of the onset and progression of TTTS. As twin pregnancies tend to be associated with preterm labor, especially after the mid-trimester, uterine contractions associated with the large uterus may play some role in the progressive development of TTTS [14-16]. The AF value in the group with TTTS developing at < 2 weeks seemed to be larger than that in the ≥ 2 weeks group, but it failed to reach significance (P = 0.34). The small sample size of this study may be one reason for the current results. Therefore, a larger prospective study is needed to clarify the possible mechanisms of TTTS development.
In conclusion, we could not identify any significant differences in the clinical histories of patients with TTTS developing at < 2 and ≥ 2 weeks in MD twin pregnancy. A larger study is needed.
| References | ▴Top |
- Lewi L, Lewi P, Diemert A, Jani J, Gucciardo L, Van Mieghem T, Done E, et al. The role of ultrasound examination in the first trimester and at 16 weeks' gestation to predict fetal complications in monochorionic diamniotic twin pregnancies. Am J Obstet Gynecol. 2008;199(5):493 e491-497.
- Thorson HL, Ramaeker DM, Emery SP. Optimal interval for ultrasound surveillance in monochorionic twin gestations. Obstet Gynecol. 2011;117(1):131-135.
doi pubmed - Carver A, Haeri S, Moldenhauer J, Wolfe HM, Goodnight W. Monochorionic diamniotic twin pregnancy: timing and duration of sonographic surveillance for detection of twin-twin transfusion syndrome. J Ultrasound Med. 2011;30(3):297-301.
pubmed - Berghella V, Kaufmann M. Natural history of twin-twin transfusion syndrome. J Reprod Med. 2001;46(5):480-484.
pubmed - Sebire NJ, Souka A, Skentou H, Geerts L, Nicolaides KH. Early prediction of severe twin-to-twin transfusion syndrome. Hum Reprod. 2000;15(9):2008-2010.
doi pubmed - Jain V, Fisk NM. The twin-twin transfusion syndrome. Clin Obstet Gynecol. 2004;47(1):181-202.
doi - Quintero RA, Morales WJ, Allen MH, Bornick PW, Johnson PK, Kruger M. Staging of twin-twin transfusion syndrome. J Perinatol. 1999;19(8 Pt 1):550-555.
doi pubmed - Elliott JP, Urig MA, Clewell WH. Aggressive therapeutic amniocentesis for treatment of twin-twin transfusion syndrome. Obstet Gynecol. 1991;77(4):537-540.
pubmed - Hiraizumi Y, Suzuki S, Satomi M, Takeshita T. Optimal interval for ultrasound surveillance in monochorionic twin gestations. Obstet Gynecol. 2011;117(5):1226-1227; author reply 1227.
doi pubmed - Van Mieghem T, Eixarch E, Gucciardo L, Done E, Gonzales I, Van Schoubroeck D, Lewi L, et al. Outcome prediction in monochorionic diamniotic twin pregnancies with moderately discordant amniotic fluid. Ultrasound Obstet Gynecol. 2011;37(1):15-21.
doi - Nakayama S, Ishii K, Kawaguchi H, Yamamoto R, Murata M, Hayashi S, Mitsuda N. Perinatal complications of monochorionic diamniotic twin gestations with discordant crown-rump length determined at mid-first trimester. J Obstet Gynaecol Res. 2014;40(2):418-423.
doi pubmed - Yamamoto R, Ishii K, Muto H, Kawaguchi H, Murata M, Hayashi S, Matsushita M, et al. The use of amniotic fluid discordance in the early second trimester to predict severe twin-twin transfusion syndrome. Fetal Diagn Ther. 2013;34(1):8-12.
doi pubmed - Gul A, Aslan H, Polat I, Cebeci A, Bulut H, Sahin O, Ceylan Y. Natural history of 11 cases of twin-twin transfusion syndrome without intervention. Twin Res. 2003;6(4):263-266.
pubmed - Murata M, Ishii K, Taguchi T, Mabuchi A, Kawaguchi H, Yamamoto R, Hayashi S, et al. The prevalence and clinical features of twin-twin transfusion syndrome with onset during the third trimester. J Perinat Med. 2014;42(1):93-98.
doi pubmed - Takahashi Y, Iwagaki S, Nakagawa Y, Kawabata I, Tamaya T. Uterine contractions increase fetal heart preload. Ultrasound Obstet Gynecol. 2003;22(1):53-56.
doi pubmed - Takahashi Y, Iwagaki S, Nakagawa Y, Kawabata I, Tamaya T. Uterine contractions might increase heart preload in the recipient fetus in early-onset twin-twin transfusion syndrome: an ultrasound assessment. Prenat Diagn. 2004;24(12):977-980.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.