| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Original Article
Volume 3, Number 1, February 2014, pages 30-34
The Efficacy of Membrane Sweeping at Term and Effect on the Duration of Pregnancy: A Randomized Controlled Trial
Tarik Y. Zamzamia, b, Nawal S. Al Senania
aDepartment of Obstetrics and Gynecology, King Abdulaziz University Hospital, Jeddah, Kingdom of Saudi Arabia
bCorresponding author: Tarik Y. Zamzami, Department of Obstetrics and Gynecology, King Abdulaziz University Hospital (KAUH), P.O. Box 80215 Jeddah 21589, Kingdom of Saudi Arabia
Manuscript accepted for publication January 17, 2013
Short title: Membrane Sweeping at Term
doi: https://doi.org/10.14740/jcgo225w
| Abstract | ▴Top |
Background: This study aimed to determine the efficacy and safety of membrane sweeping on the duration of pregnancy at term and induction rate. The study design was a randomized controlled trial.
Method: The study conducted at the King Abdulaziz University Hospital, Jeddah, Saudi Arabia, from January 1, 2011 to January 1 2012. One hundred and sixty women with uncomplicated pregnancy attending the antenatal clinic and delivery room were randomized to membrane sweeping (study group, n = 80) or no sweeping (control group, n = 80) at 38 weeks of gestation.
Results: Most of the women who underwent membrane sweeping entered spontaneous labor (90 vs. 75%), with a significant difference in mean gestational age (39.5 ± 0.9 vs. 40.0 ± 1.2, P = 0.004). The overall incidence of pregnant women at 41 week gestation was 10 % in women who underwent membrane sweeping and 25% in the controls (OR 3.0, 95% CI 1.2 - 7.3, P = 0.01). The induction rate was less in study compared to control group (10 % vs. 25%; P = 0.01). There were no differences in the incidence of cesarean delivery, or maternal or fetal morbidity between the two groups.
Conclusion: Sweeping of the membranes at term is safe and reduces the incidence of post-date gestation. Most women required only a single cervical sweeping.
Keywords: Membrane sweeping; Induction; Cesarean section
| Introduction | ▴Top |
Membrane sweeping is one of the mechanical methods of induction of labor at term in women with and without 1 prior cesarean section. The primary aim is to initiate labor and or to improve favorability of the cervix by increasing local production of prostaglandins [1, 2]. It is an effective mean of induction in uncomplicated term pregnancy, but less efficient than other methods such as the use of oxytocin, prostaglandins and amniotomy [3, 4]. This procedure is a conservative and a non invasive approach, which could be performed in the situations where the indication to induce labor is not immediate or urgent for intervention. Therefore, membrane sweeping may hasten the onset of labor and reduces the number of pregnant women continuing beyond 41 weeks and the need for formal labor induction. Maternal side effects such as discomfort and mild vaginal bleeding are not uncommon but no evidence of increased maternal and fetal infection [1, 5]. The aims of this study were: 1), to evaluate the safety and efficacy of membrane sweeping at term; and 2), to determine the induction rate of labor among women who undergo membrane sweeping.
| Methods | ▴Top |
This was a randomized controlled trial conducted at the King Abdulaziz University Hospital, Jeddah, Saudi Arabia, from January 1, 2011, to January 1, 2012. Women with uncomplicated pregnancy who were attending the antenatal clinic were enrolled if they met the following criteria: singleton pregnancy, cephalic presentation, and anticipated vaginal delivery. Exclusion criteria were; indications for induction of labor, indications for cesarean section, and contraindications to membrane sweeping, such as multiple gestation, placenta previa, placental abruption, history of preterm delivery, vasa previa, active cervical infection, Mullerian anomalies, severe fetal anomalies and active herpes infection. The study was approved by the Biomedical Ethics Research Committee and Human Investigation “according to principles of Helsinki Declaration” at King Abdulaziz University (HA-02-J-008).
Before randomization, women who met the inclusion criteria received counseling about their participation in the study. Two hundred and forty women were legible for the study, 80 women refused participation and were excluded; 160 agreed to participate and provided written informed consent from all participants. These women were assigned randomly at 38 weeks to membrane sweeping “study group” or no membrane sweeping or intervention “control group” [1, 6]. Gestational age was base on the women’s last menstrual period and confirmed by early ultrasound scans. The assignment was by using computer-generated numbers, with allocation concealed in opaque sealed envelopes that were drawn in order. All membrane sweeping group was performed by one clinician investigator and women allocated to control group received routine monitoring; in each case, the cervix was dilated and the health provider swept a finger in a 360° manner inside the cervix, thereby separating the lower uterine segment from the amniotic sac. If the cervix was closed, it was massaged digitally [6, 7]. In the study group modified Bishop scoring were determine as the following; cervical dilatation, effacement and fetal station [8]. All pregnant women “both groups” who did not enter spontaneous labor or remaining undelivered at 41 weeks gestation were being admitted and underwent for induction of labor.
On admission to labor room and at delivery, the indication for admission, estimated gestational age at delivery by early ultrasound scans done, Modified Bishop Score, duration of labor, mode of delivery, and birth weight were determined and recorded. The primary outcome measures were the interval from membrane sweeping to onset of labor, and the proportion of pregnant women whose gestation at 41 weeks were determine in both groups. Others outcome measures were the incidence of prelabor ruptured membranes (PROM), labor induction rate, meconium stain amniotic fluid, mode of delivery, Macrosomia (birth weight ≥ 4 kg), and maternal and fetal outcomes. Differences in demographics, obstetric outcomes and complications were analyzed. After 60 women had been allocated to each group, the sample size was estimated indicated that 112 women would be necessary to show that membrane sweeping decreases post-date pregnancy at 41week by 15% (using alpha error = 0.05, beta error = 0.2, power = 80%). The study was done in a way whereby CONSORT criteria were fulfilled, and give an a priori power calculation to enlarged the study population and analysis was by intention-to-treat. The trial flow diagram is shown in Figure 1.
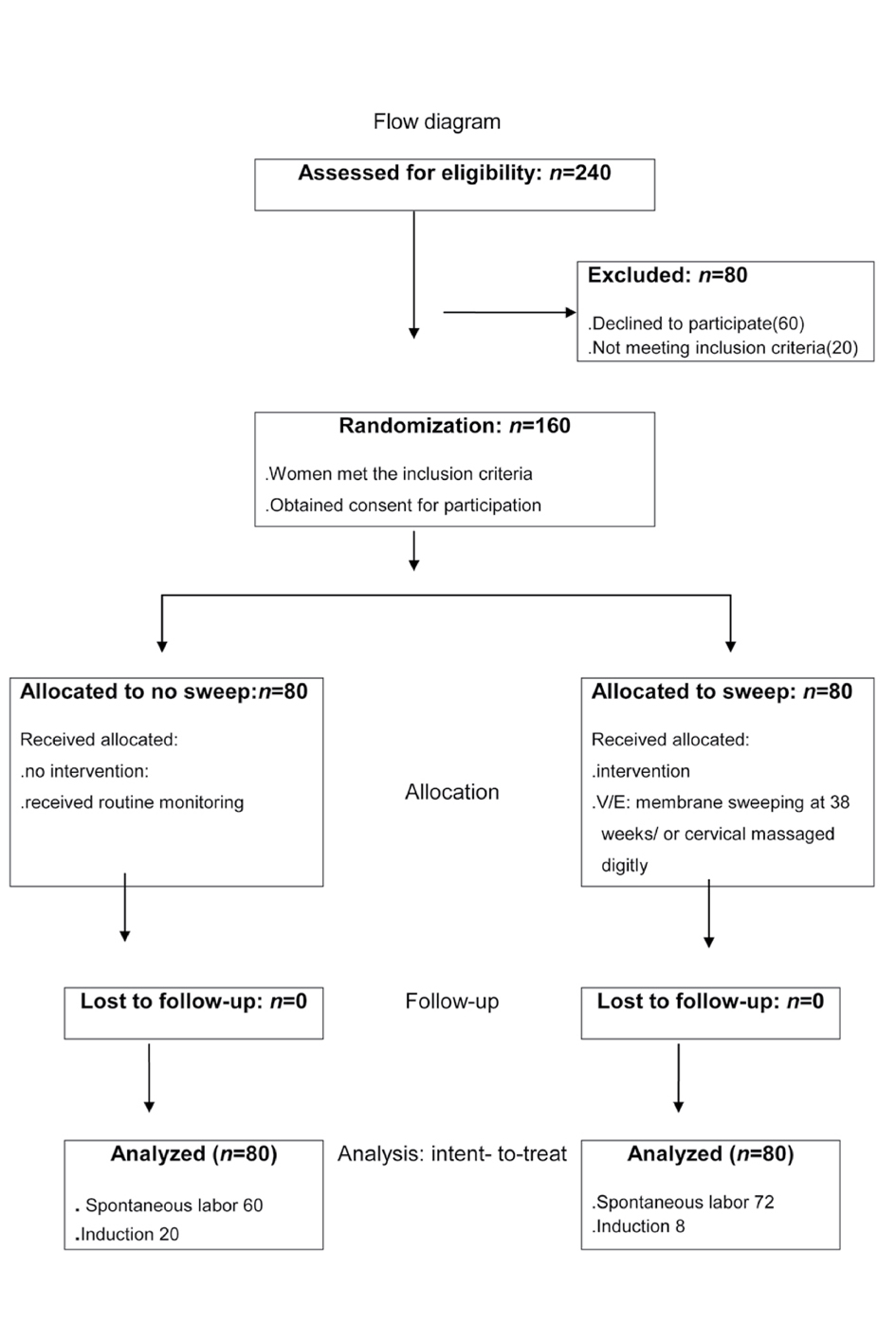 Click for large image | Figure 1. Flow diagram. |
Statistical analysis was performed using SPSS-PC for windows, version 18. Data were expressed as the percentage or means ± SD. Student t-test was used for continuous variables and the chi-square test or Fisher exact test for categorical data. Odds ratio (ORs) and the 95% confidence intervals (CIs) were calculated. P values < 0.05 were considered statistically significant.
| Results | ▴Top |
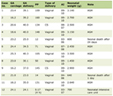
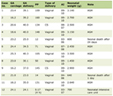
During the study period, 240 women were eligible for inclusion in the study. Eighty women decline to participate; the remaining 160 were randomized for either membrane sweeping at 38 weeks of gestation (study group, n = 80) or no membrane sweeping (control group, n = 80). The maternal characteristics presented in Table 1 showed no differences between the two groups in the following variables: percentage of primigravida, and mean age, gravidity, parity, gestational age, and body mass index (BMI). The mean ± SD of Bishop score initially was (2.0 ± 1.1), compared to cervical Bishop-score on admission in labor was improved and greater than the initial cervical assessment obtained antenatally (4.0 ± 1.3 vs. 2.0 ± 1.1, P = 0.001). Majority of women had 1 membrane sweeping 65 (81.3%) went into spontaneous onset of labor between 39 - 40 week, and 15 (18.75%) women had ≥ 2 membrane sweeping 7 (8.75%) of them went into spontaneous onset of labor < 41 weeks and 8 (10%) needs induction of labor at 41 weeks gestational age. The labor induction rate (25% vs. 10%) was greater in the control cases (OR, (95% CI): 3 (1.2 - 7.3); P = 0.01). There were no differences in obstetric complications (prior 1 cesarean section in current pregnancy, and PROM) between the two groups Table 2. The gestational age on admission in labor based on early ultrasound (mean ± SD) was less and statistically significant in study compared to control group. The less pregnancy duration and more spontaneous onset of labor in the study were statistically significant. The incidence of meconium stained amniotic fluid was higher in the controls (25% vs. 5%; OR (95% CI): 5 (1.8 - 14); P = 0.001). Birth weight, incidence of Macrosomia and duration of labor were greater and statistically significantly in the control group. There were no differences in incidence of cesarean delivery, or maternal or fetal complications between the two groups Table 3.
 Click to view | Table 1. Maternal Characteristics |
 Click to view | Table 2. Obstetric Complications |
 Click to view | Table 3. Maternal and Fetal Outcomes |
| Discussion | ▴Top |
Several studies of the effectiveness of membrane sweeping have produced inconsistence results. A recent Cochrane review reported that routine use of membrane sweeping from 38 weeks onwards does not seem to have clinically important benefits [5]. However, the efficacy of membrane sweeping is expected to be low at an earlier gestational age, and the major concern are pregnancies that extend beyond 41 weeks of gestation with unfavorable cervix [9]; de Miranda et al [7] noted that the Cochrane review included studies with relatively small sizes, and heterogeneity between the trial results outcome.
Outpatient membrane sweeping at term is used to prevent post-term pregnancies and associated with a reduction in pregnancy duration. Data in the literature indicate that cervical sweeping of the membranes performed antenatally can reduce the time to spontaneous onset of labor [1, 2, 5]. Tan et al [10] reported that membrane sweeping combined with other induction methods has synergistic effects that can lead to reduction of the interval before induction of labor. This intervention has been shown to increase endogenous production prostaglandins, phospholipase A and oxytocin, which help to ripen the unfavorable cervix and reduced need for supplemental oxytocin in women in active labor [2, 4, 9]. The present study shows a significant decrease in the incidence of post-date pregnancy at 41weeks, and with a lower induction rate (10% vs. 25%; P = 0.01) and a significant decrease in mean gestational age (39.5 ± 0.9 weeks versus 40.0 ± 1.2 weeks; P = 0.004) compared with the controls.
A single membrane sweeping procedure at 38 - 40 weeks of gestation is effective and no significant difference has been found in the percentage of women who enter spontaneous labor within 7 days or before 41 weeks [1, 5, 9]. The effect of membrane sweeping might be enhanced if the procedure is performed immediately before the onset of labor [10]. In the present study, sweeping of the membranes was performed weekly at 38 weeks onwards improved an unfavorable Bishop score on women admission in labor (4.0 ± 1.3 vs. 2.0 ± 1.1, P = 0.001). Most of the women (81.3%) enter spontaneous labor following a single membrane sweeping, and delivered 1 week earlier than the control group. Few women in the study needed repeated membrane sweeping. The precise effect of repeat membrane sweeping is not well understood. Chanrachakul et al [11] reported that serial membrane sweeping in nulliparous women is not useful, whereas de Miranda et al [7] reported that weekly sweeping places women in a prelabor state in which irregular uterine contractions have a cervical ripening effect, and improves the Bishop score on admission [4, 12]. Several studies have shown that fewer women eventually need induction for pregnancy beyond 41 weeks if membrane sweeping is performed antenatally [1, 2, 4, 7]. This finding is consistent with the present study (10 vs. 25%; P = 0.01). Women in the sweeping membranes group reported and felt discomfort pain during vaginal examination and after the intervention, the other side effects attributable to sweeping membranes such as slight bleeding is not uncommon.
Limitation of this study is that the number of women with prior 1 cesarean section is small, and need further study to determine the efficacy and safety of the membranes sweeping with 1 prior cesarean section in the future.
Sweeping of the membranes is safe, relatively noninvasive and improved unfavorable cervix at term, but has less predictable results than other methods of labor induction. There is no evidence that the ancillary outpatient procedure increases risk of maternal or fetal infection although this was not part of their study [1, 5, 7]. In conclusion: Sweeping of the membranes at term is safe and reduces the incidence of post-date gestation. Most women required only a single cervical sweeping.
Acknowledgments
This project was funded by the Deanship Scientific Research (DSR), King Abdulaziz University, Jeddah, under grant no. (1432/140/7). The authors, therefore, acknowledge with thanks DSR technical and financial support.
Disclosure of Benefit
Authors have no conflict of interests and the work was not supported or funded by any drug company.
| References | ▴Top |
- Mozurkewich EL, Chilimigras JL, Berman DR, Perni UC, Romero VC, King VJ, Keeton KL. Methods of induction of labour: a systematic review. BMC Pregnancy Childbirth. 2011;11:84.
doi pubmed - Yildirim G, Gungorduk K, Karadag OI, Aslan H, Turhan E, Ceylan Y. Membrane sweeping to induce labor in low-risk patients at term pregnancy: a randomised controlled trial. J Matern Fetal Neonatal Med. 2010;23(7):681-687.
doi pubmed - Wong SF, Hui SK, Choi H, Ho LC. Does sweeping of membranes beyond 40 weeks reduce the need for formal induction of labour? BJOG. 2002;109(6):632-636.
doi pubmed - Dare FO, Oboro VO. The role of membrane stripping in prevention of post-term pregnancy: a randomised clinical trial in Ile-lfe, Nigeria. J Obstet Gynaecol. 2002;22(3):283-286.
doi pubmed - Boulvain M, Stan C, Irion O. Membrane sweeping for induction of labour. Cochrane Database Syst Rev. 2005;(1):CD000451.
pubmed - Hill MJ, McWilliams GD, Garcia-Sur D, Chen B, Munroe M, Hoeldtke NJ. The effect of membrane sweeping on prelabor rupture of membranes: a randomized controlled trial. Obstet Gynecol. 2008;111(6):1313-1319.
doi pubmed - de Miranda E, van der Bom JG, Bonsel GJ, Bleker OP, Rosendaal FR. Membrane sweeping and prevention of post-term pregnancy in low-risk pregnancies: a randomised controlled trial. BJOG. 2006;113(4):402-408.
doi pubmed - Osmundson SS, Ou-Yang RJ, Grobman WA. Elective induction compared with expectant management in nulliparous women with a favorable cervix. Obstet Gynecol. 2010;116(3):601-605.
doi pubmed - Putnam K, Magann EF, Doherty DA, Poole AT, Magann MI, Warner WB, Chauhan SP. Randomized clinical trial evaluating the frequency of membrane sweeping with an unfavorable cervix at 39 weeks. Int J Womens Health. 2011;3:287-294.
pubmed - Tan PC, Jacob R, Omar SZ. Membrane sweeping at initiation of formal labor induction: a randomized controlled trial. Obstet Gynecol. 2006;107(3):569-577.
doi pubmed - Chanrachakul B, Suthutvoravut S, Sangthawan M, Herabutya Y. Effect of lower uterine segment sweeping on progress of labor in nullipara. J Med Assoc Thai. 2001;84(11):1582-1586.
pubmed - Hamdan M, Sidhu K, Sabir N, Omar SZ, Tan PC. Serial membrane sweeping at term in planned vaginal birth after cesarean: a randomized controlled trial. Obstet Gynecol. 2009;114(4):745-751.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.