| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website http://www.jcgo.org |
Case Report
Volume 3, Number 1, February 2014, pages 42-49
One Hundred and Fourteen Days of Somatic Support in a Severely Brain Injured Pregnant Woman: Case Report and Review of the Literature
Henry Adekolaa, b, c, Zaid Al-Wahaba, Leonard Sudakina, Karoline Pudera, b, Bernard Gonika, b
aDepartment of Obstetrics and Gynecology, Wayne State University School of Medicine, Detroit, MI, USA
bDivision of Maternal Fetal Medicine, Sinai Grace Hospital/Wayne State University School of Medicine, Detroit, MI, USA
cCorresponding author: Henry Adekola, Division of Maternal Fetal Medicine, Hutzel Women’s Hospital/Wayne State University School of Medicine, 3990 John R, Detroit MI, 48201, USA
Manuscript accepted for publication October 1, 2013
Short title: Somatic Support
doi: https://doi.org/10.14740/jcgo197w
| Abstract | ▴Top |
The management of a previable pregnancy complicated by severe brain injury raises the question of whether to provide somatic support in order to maintain the pregnancy or not. Obstetricians who encounter this clinical scenario are faced with emotional, medical and ethical complexities, which require multidisciplinary input. A 19-year-old woman with an unremarkable medical history suffered severe brain injury and remained in a persistent vegetative state following a gunshot wound to the neck. She was discovered to be 15 weeks pregnant during resuscitative efforts. Following consultation with her family and power of attorney it was agreed to continue somatic support in order to maintain the pregnancy. A literature review to determine the best evidence based care from a multidisciplinary perspective is performed addressing issues of ethics, simulation and management of changes in maternal physiology, as well as pregnancy outcomes based on the neurological sequelae following severe brain injury. Previable pregnancies complicated by severe brain injury may be maintained until viability. Based on limited data, the obstetric outcomes may differ depending on whether the neurological sequelae are brain death or a persistent vegetative state. This management should be performed following consultation with the patient’s power of attorney in conjunction with the ethics committee and legal department of the hospital. Maternal physiological changes of pregnancy must be considered for successful somatic support.
Keywords: Previable pregnancy; Severe brain injury; Brain death; Persistent vegetative state
| Introduction | ▴Top |
Consciousness can be defined as the ability to experience or to feel, wakefulness, having a sense of selfhood, and the executive control system of the mind [1]. Unconsciousness, which is the opposite, consists of 3 forms: coma, brain death and persistent vegetative state (PVS) [2, 3]. All 3 forms can be caused by traumatic and atraumatic (for example, cerebrovascular accident, hypoxia, hypothermia, hypoglycemia intoxication and so on) brain injury, with the latter usually associated with poorer outcomes than the former [2, 3].
Coma is a state in which the patient cannot be aroused by any stimulus, however vigorous or painful. Thus, the patient in coma shows no response to any external stimulus or inner need and lacks both wakefulness and awareness. Brain death is the unequivocal and irreversible loss of all brain function. These patients have lost all brain stem functions and cranial nerve reflexes and are irreversibly comatose. In contrast to this, patients in a persistent vegetative state though lacking cerebral function still possess brain stem function for example swallowing and respiratory control. Clinically they can be observed to be awake as they still possess sleep-wake cycles. Table 1 summarizes the difference between these 3 forms of unconsciousness [2, 3].
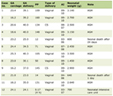 Click to view | Table 1. Overview of the Clinical Features of Coma, Persistent Vegetative State, and Brain Death [2] |
It is unlikely that a pregnancy well beyond viability will be maintained following a maternal neurologic transition from consciousness to a persistent vegetative state or a brain dead status secondary to a severe brain injury as a perimortem cesarean section is usually performed as part of the resuscitative efforts. However the same cannot be said for a previable pregnancy. The question of whether or not to provide somatic support may be associated with emotional, medical and ethical complexities, which require multidisciplinary input.
We present a case of an early second trimester pregnancy complicated by maternal PVS due to a catastrophic brain injury following a gunshot wound to the neck. In this case we describe the different medical modalities aimed at supporting the fetus via maintenance of maternal homeostasis and address the pertinent ethical and medical issues associated with this very rare complex obstetric situation.
| Case Report | ▴Top |
A 19-year-old African American female with an unremarkable medical, surgical or obstetric history was brought into the emergency room within 3 - 4 min after suffering a gunshot injury to the neck during a drive-by shooting. She was observed to be unresponsive and exsanguinating from the injury site. The bleeding was abated by insertion and inflation of a Foley catheter at the bleeding site. Cardiopulmonary resuscitation was performed following a finding of complex sinus bradycardia. Endotracheal intubation was performed as a part of the resuscitation effort. A 15-week pregnancy was discovered during initial assessment. She received epinephrine and atropine during resuscitative efforts. During surgical neck exploration a massive hematoma was found in the neck encircling the right internal jugular vein and a paracervical hematoma posterior to the esophagus. Tracheostomy and percutaneous endoscopic gastrostomy tubes were placed to facilitate breathing and enteral feeding respectively. Computer tomography (CT) of the neck showed a comminuted fracture of C6 with posterior displacement of a fragment into the cervical canal with spinal cord compression and occlusion of the left vertebra artery. A computer tomography scan of the brain showed global cerebral edema with herniation and radiological evidence of hypoxic ischemic encephalopathy.
Following initial resuscitative and surgical care a full systemic examination revealed an unresponsive young pregnant female with spontaneous eye opening, intact corneal and pupillary reflexes, a weak gag reflex and absent rectal tone. The patient was thus designated as being in the vegetative state from acute severe cerebral hypoperfusion with quadriplegia secondary to the gunshot wound (GSW) to the neck. She required ventilatory support in the surgical intensive care unit (SICU).
The presence of a previable pregnancy in a patient in the vegetative state prompted consultation of the hospital ethics committee and legal department. A meeting to determine direction of care was convened with the patient’s family members, maternal-fetal medicine specialist and the primary care team (SICU), and ethics committee. During this meeting it was discovered that the pregnancy was concealed. After extensive counseling about patient’s medical condition the family elected to continue life support and insisted that every effort be made to continue the pregnancy. This decision was made with the understanding of the increased risk for adverse pregnancy outcome secondary to maternal-fetal hypoxia, multiple medication and radiation exposures, the anticipated multiple maternal infections and the risk of extreme prematurity. The patient’s family elected her mother as legal guardian and power of attorney for all future decisions. The primary management team (SICU) was counseled to balance the risk-benefits of further radiological exposure and to carefully select maternal medications.
Prenatal labs were within normal limits except for a chromosomal aneuploidy quad screen that placed the fetus at a 1:92 risk for Down syndrome. Her legal guardian declined an amniocentesis and an anatomy ultrasound performed at 19 weeks gestational age revealed no classic ultrasound findings (“soft markers”) consistent with Down syndrome or any other anomalies except for a single umbilical artery. Weekly clinical assessment was performed by the maternal-fetal medicine unit with daily fetal heart tones check, which was changed to twice daily non-stress tests at 30 weeks gestational age. The patient was nursed with left abdominal tilt at all times to maximize uteroplacental perfusion.
Hospital days (HDs) 5, 25, 35 and 53 were complicated by maternal fever secondary to recurrent urinary tract infection and then bacteremia with Enterococcus species that was managed with appropriate antibiotics and subsequent administration of urologic antibiotic suppression. She required multiple bronchoscopies to suction mucus plugs which led to left sided lung collapse. On HD 81 she received a blood transfusion secondary to anemia. After an episode of complicated staphylococcal pneumonia, antenatal corticosteroids for fetal lung maturity were administered on HD 111 (31 weeks gestation).
Spontaneous rupture of membranes with the onset of preterm labor was identified at 31 weeks and 2 days gestation. Continuous fetal monitoring was commenced and 8 hours after she was in the second stage of labor. A Simpson forcep was used to shorten the second stage of labor after the fetal head descended to +3 station. A live male infant with a birth weight of 1,740 g with an Apgar score of 9 in 5 min was delivered. There were no dysmorphologic features observed. Umbilical arterial gas values were: pH 7.08; bases excess -7.0 mmol/L; pO2 20 mmHg; and pCO2 89 mmHg. The neonate did not require respiratory support and his neonatal course was uneventful. Custody of the infant was given to the patient’s mother.
The patient was transferred to a long-term care facility on HD 120 where she died of respiratory complications 2 months before her son’s 6th birthday. Her son has so far achieved all developmental milestones and has no evidence of neurological deficits.
| Discussion | ▴Top |
The incidence of pregnancy associated with a gravida in the vegetative state is unknown. What is known is that like in our patient, 7% of all pregnancies are complicated by traumatic injury while trauma is responsible for < 1% of hospitalizations in pregnancy [4]. In addition, trauma accounts for almost 4% of maternal mortality and 9% of fetal mortality [5]. However, on reviewing the literature (including this case), there is an equal frequency of traumatic and atraumatic etiologies for the occurrence of PVS in a pregnant woman [4-21]. As expected, there is a disparity favoring an atraumatic etiology in pregnant patients with brain death [22-31].
The physician faced with the dilemma of pregnancy in a patient in either the vegetative state or brain dead must consider whether to 1) attempt delivery of the fetus if past the age of viability; 2) immediately discontinue life support measures with the knowledge that this will lead to fetal death; or 3) like in our case continue full life support measures in an attempt to prolong the pregnancy with the aim of achieving further fetal maturity. Unfortunately, the wishes of the victim of this catastrophic event are almost never known. Thus the decision of which path to follow in the care of these patients should be taken after careful and exhaustive consultation with her family, the hospital ethics and legal departments. Some authors who have addressed this issue in brain dead individuals recommend involving the next of kin-usually the father of the fetus in the decision making [22, 32, 33]. Others have proposed a hierarchy for surrogate decision in descending order of: 1) an individual designated verbally or in writing in an advance directive or durable power of attorney for healthcare decisions; 2) a guardian authorized by the courts; 3) the spouse; 4) an adult child or adult children of the patient; 5) parent or parents; 6) an adult sibling; and 7) any other blood relative [13]. In a situation when there is a difference of opinion on how this patient should be managed due to family conflict or rift, the legal department of the hospital should be involved with recourse to the judicial system to nominate a surrogate decision maker.
In the event that that the family or surrogate decision-makers choose to continue life support measures and continue the pregnancy, it is imperative that the providers determine whether the brain injured unconscious patient is brain dead or in a vegetative state. This is important because, unlike the patient who is brain dead, the patient in PVS has the possibility of recovery. Data from the multi-society task force on PVS show that 52% of adults recover consciousness within 1 year, with a majority of these occurring within the first 6 months. Recovery after 6 months is usually unlikely [2, 3]. Thus somatic support in a pregnant woman in a persistent vegetative state is intended to preserve basic body functions with the possibility (although sometimes remote) of maternal recovery in addition to preservation and or maturation of the unborn fetus. This is in contrast to the pregnant woman who is brain dead for whom somatic support is only advantageous to the fetus [34]. Another reason to differentiate between PVS and brain death is that based on published literature, there is a significantly longer interval between maternal brain injury and delivery, which in turn results in higher gestational ages and birth weights at delivery when the PVS group is compared to the brain dead group [9]. The aforementioned information should be explained to patient’s family or surrogate decision-maker in order for them to make an informed decision.
Based on the type of neuropathology, a pregnancy complicated by PVS generally may require less somatic support than its brain dead counterpart. However PVS during pregnancy may require medical management close to the care received by a pregnancy complicated by brain death. This case was complicated by transection of the spinal cord at the cervical spine level, compromising innervation of the maternal diaphragm. Thus explain the need for prolonged mechanical ventilation.
In providing somatic support, the normal physiologic changes of pregnancy should be considered and attempted to be replicated. Changes in maternal physiology for consideration are summarized in Table 2 and addressed below.
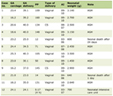 Click to view | Table 2. Important Maternal Physiologic Changes in Pregnancy [35, 36, 57, 58, 60] |
Cardiovascular system
In a normal pregnancy the cardiac output is increased by 50% from the non-pregnant state with the uterus receiving about 30% of this increment [35, 36]. On admission to the emergency room this patient required cardiopulmonary resuscitation due to a finding of complex sinus bradycardia, which is usually associated to hypotension. Hemodynamic support is critical to maintaining adequate uteroplacental perfusion, which in turn is vital to fetal survival as uterine blood flow lacks auto regulation. The management of hypotension will require intravenous fluid infusion (including blood transfusion) and possible inotropic medications in addition to vasopressors. The American Heart Association guideline for cardiopulmonary resuscitation does not modify or change the type or dosage of medications used in resuscitation of pregnant women [37]. In addition, defibrillators can be utilized without significant complication to the fetus [38]. Thus intravascular volume should be maintained and central venous pressure or pulmonary artery occlusion pressure measurements may be utilized for its surveillance [39]. The PVS patient should be nursed with a left abdominal tilt to avert supine hypotension syndrome. The possibility of low oncotic pressure due to suboptimal nutrition should be kept in mind and as such volume expansion should be with a combination of crystalloids and colloids [40].
Respiratory system
Respiratory support in the mode mechanical ventilation may be pivotal to supporting life in patients like in this index case. Usually the preservation of brain stem activity dictates that PVS patients require less respiratory support than their brain dead counterparts. Our patient required mechanical ventilatory support due to the mechanism of her injury and respiratory complications, which led to lung collapse. Although the fetus possesses mechanisms to avert hypoxia, adequate maternal oxygenation is pivotal as threshold for maternal hypoxia is significantly increased in pregnancy due to increased oxygen requirement and minute ventilation and reduced functional residual capacity [35, 36]. It is also important to consider and maintain the fetal CO2 diffusion gradient by maintaining the maternal PaCO2 at between 28 - 31 mmHg [41] which is lower than what is expected in non-pregnant individuals [42]. The risk of respiratory alkalosis which can lead to uterine hypoperfusion must be taken into consideration [43].
Endocrine system
Panhypopituitarism due to disruption of the hypothalamic-pituitary axis is the usual cause of an abnormal endocrine milieu in the severely brain injured individuals who later progress to brain death [39] or a persistent vegetative state [10]. This may lead to reduced production of antidiuretic hormone (ADH), cortisol and thyroxine. Central diabetes insipidus (CDI) is a common endocrine anomaly in both PVS and brain dead patients receiving somatic support [10, 39]. Polyuria and hypernatremia from CDI if uncorrected may result in constriction of intravascular volume which in turn may lead to uteroplacental underperfusion and its attendant complications. This can be corrected by administration of vasopressin intranasally, intramuscularly or intravenously. Correction of hypothyroidism to avert abnormal brain development cannot be overemphasized and this correction with that of reduced serum cortisol by hormone replacement should be guided by measurement of thyroid and adrenal function. In replacing cortisol it may be safer to utilize hydrocortisone or prednisone instead of betamethasone and dexamethasone as these glucocorticoids are not inactivated by placental 11β-hydroxysteriod dehydrogenase type 2 enzyme [44, 45] and prolonged exposure to them have been associated reduced fetal birth weight [46, 47], as well as adverse metabolic [48, 49] and neurologic [50, 51] effects in both animal and human studies.
Nutrition
Nutritional support is an integral part of the somatic management of these types of patients. Sampson and Petersen reported a weight loss of almost 20 lbs in the first 4 weeks of hospitalization of a pregnant PVS patient [18]. The Institute of Medicine recommends that a normal pregnancy should achieve a weight gain of 11.5 - 16 kg (25 - 35 lbs) [52]. Furthermore, some authors based on clinical experience have advocated for daily calorie intake of 3,000 - 4,000 kcal to avert nutritional deficiency in these patients [53]. Nutritional support can be achieved by enteral (which was performed in our patient-percutaneous entero gastrostomy), parenteral or both. Thus based on the aforementioned, daily weight measurement should be part of supportive care. Supplementation of vitamins and trace elements is important as shown in our patient whose care was complicated by anemia.
Infectious morbidity and temperature regulation
Fever usually heralds this complication. However hypothalamic damage may be the cause of a labile hyperthermia. Nonetheless, the potential source and type of infection should be aggressively investigated. As with most intensive care type patients, urinary tract infection and pneumonia are the most common infections [54]. These morbidities affected our patient. Adverse neurological fetal effects of hyperthermia are well known [55] and as such antipyretics as well cooling blankets in addition to pregnancy-appropriate antimicrobials should be administered to these patients. Although hyperthermia can occur due to hypothalamic dysfunction in these patients, hypothermia is far more common and this has been shown to be associated with altered breathing pattern and fetal bradycardia in animal models [56]. This can be managed with warming blankets which have been shown to reverse the aforementioned adverse fetal effects in the same animal studies [56].
Other measures of optimizing fetal outcomes
It is important to perform a detailed anatomy ultrasound scan to determine the presence or absence of fetal anomalies and to also examine for features that might be associated with chromosomal abnormalities. This should be followed by appropriate screening and diagnostic studies. These findings may alter the request to maintain or prolong pregnancy if viability has not been attained. Regular fetal monitoring by nonstress testing should be performed on daily basis when the fetus achieves viability. In addition the providers may decide to administer antenatal corticosteroids at viability or when there is an increased risk for preterm delivery like in this case when the patient developed pneumonia. Routine gestational age indicated laboratory testing as in the conscious patient should be performed as specific optimizing interventions may be indicated based on these results.
Pregnancy being a hypercoagulable state due to alterations in certain clotting factors [57, 58] increases the frequency of venous thromboembolism 5 times more than the non-pregnant woman [59, 60]. Thus the need for adequate prophylactic anticoagulation in the recumbent immobile brain dead pregnant woman or one in a persistent vegetative state cannot be overemphasized.
Conclusion
To our knowledge this is only the 19th reported case of a pregnancy complicated by PVS and the 6th in which a vaginal delivery was performed. Given the paucity of available data, in this report we detail interventional strategies based on literature review and recognized pregnancy-specific physiologic considerations. When faced with this clinical scenario, the physician must determine whom the designated surrogate decision-maker is and if the patient’s wishes were known prior to the event. The form of unconsciousness must also be determined as data in the literature show significant differences in maternal and fetal outcomes based on whether the brain injury led to PVS or brain death. The obstetric team in conjunction with the intensive care unit should attempt to maintain and or simulate pregnancy physiologic homeostasis.
This case as well as others before it, shows that with optimal somatic support, it is possible to maintain a previable pregnancy and achieve delivery (albeit prematurely) with minimal short and long-term neurological disabilities in the fetus.
Conflict of Interest
Authors report no conflict of interest.
| References | ▴Top |
- GF. The psychology of conciousness: Prentice Hall; 1992.
- Medical aspects of the persistent vegetative state (1). The Multi-Society Task Force on PVS. N Engl J Med. 1994;330(21):1499-1508.
doi pubmed - Medical aspects of the persistent vegetative state (2). The Multi-Society Task Force on PVS. N Engl J Med. 1994;330(22):1572-1579.
doi pubmed - Shah KH, Simons RK, Holbrook T, Fortlage D, Winchell RJ, Hoyt DB. Trauma in pregnancy: maternal and fetal outcomes. J Trauma. 1998;45(1):83-86.
doi pubmed - Rogers FB, Rozycki GS, Osler TM, Shackford SR, Jalbert J, Kirton O, Scalea T, et al. A multi-institutional study of factors associated with fetal death in injured pregnant patients. Arch Surg. 1999;134(11):1274-1277.
doi pubmed - Abazzia C, Adamo F, Gill B, Morrison R, Volpe K, Prata J. In the name of good intentions: nurses' perspectives on caring for a pregnant patient in a persistent vegetative state. Crit Care Nurse. 2010;30(1):40-46.
doi pubmed - Ayorinde BT, Scudamore I, Buggy DJ. Anaesthetic management of a pregnant patient in a persistent vegetative state. Br J Anaesth. 2000;85(3):479-481.
doi pubmed - Ben Aderet N, Cohen I, Abramowicz JS, Becker E, Sazbon L. Traumatic coma during pregnancy with persistent vegetative state. Case report. Br J Obstet Gynaecol. 1984;91(9):939-941.
doi pubmed - Bush MC, Nagy S, Berkowitz RL, Gaddipati S. Pregnancy in a persistent vegetative state: case report, comparison to brain death, and review of the literature. Obstet Gynecol Surv. 2003;58(11):738-748.
doi pubmed - Chiossi G, Novic K, Celebrezze JU, Thomas RL. Successful neonatal outcome in 2 cases of maternal persistent vegetative state treated in a labor and delivery suite. Am J Obstet Gynecol. 2006;195(1):316-322.
doi pubmed - Diamond MP, Boehm FH, Allen G. Long term management of pregnancy in a comatose patient. J Tenn Med Assoc. 1986;79(9):557-558.
pubmed - Feldman DM, Borgida AF, Rodis JF, Campbell WA. Irreversible maternal brain injury during pregnancy: a case report and review of the literature. Obstet Gynecol Surv. 2000;55(11):708-714.
doi pubmed - Finnerty JJ, Chisholm CA, Chapple H, Login IS, Pinkerton JV. Cerebral arteriovenous malformation in pregnancy: presentation and neurologic, obstetric, and ethical significance. Am J Obstet Gynecol. 1999;181(2):296-303.
doi - Hill LM, Parker D, O'Neill BP. Management of maternal vegetative state during pregnancy. Mayo Clin Proc. 1985;60(7):469-472.
doi - Koh ML, Lipkin EW. Nutrition support of a pregnant comatose patient via percutaneous endoscopic gastrostomy. JPEN J Parenter Enteral Nutr. 1993;17(4):384-387.
doi - Landye ST. Successful enteral nutrition support of a pregnant, comatose patient: a case study. J Am Diet Assoc. 1988;88(6):718-720.
pubmed - Lucas B. Nursing care study: pregnant car-crash victim. Nurs Times. 1976;72(12):451-453.
pubmed - Sampson MB, Petersen LP. Post-traumatic coma during pregnancy. Obstet Gynecol. 1979;53(3 Suppl):2S-3S.
pubmed - Sim KB. Maternal persistent vegetative state with successful fetal outcome. J Korean Med Sci. 2001;16(5):669-672.
pubmed - Webb GW, Huddleston JF. Management of the pregnant woman who sustains severe brain damage. Clin Perinatol. 1996;23(3):453-464.
pubmed - Wong M, Apodaca CC, Markenson MG, Yancey M. Nutrition management in a pregnant comatose patient. Nutr Clin Pract. 1997;12(2):63-67.
doi pubmed - Bernstein IM, Watson M, Simmons GM, Catalano PM, Davis G, Collins R. Maternal brain death and prolonged fetal survival. Obstet Gynecol. 1989;74(3 part 2):434-437.
- Catanzarite VA, Willms DC, Holdy KE, Gardner SE, Ludwig DM, Cousins LM. Brain death during pregnancy: tocolytic therapy and aggressive maternal support on behalf of the fetus. Am J Perinatol. 1997;14(7):431-434.
doi pubmed - Dillon WP, Lee RV, Tronolone MJ, Buckwald S, Foote RJ. Life support and maternal death during pregnancy. JAMA. 1982;248(9):1089-1091.
doi pubmed - Field DR, Gates EA, Creasy RK, Jonsen AR, Laros RK, Jr. Maternal brain death during pregnancy. Medical and ethical issues. JAMA. 1988;260(6):816-822.
doi pubmed - Heikkinen JE, Rinne RI, Alahuhta SM, Lumme JA, Koivisto ME, Kirkinen PP, Sotaniemi KA, et al. Life support for 10 weeks with successful fetal outcome after fatal maternal brain damage. Br Med J (Clin Res Ed). 1985;290(6477):1237-1238.
doi - Iriye BK, Asrat T, Adashek JA, Carr MH. Intraventricular haemorrhage and maternal brain death associated with antepartum cocaine abuse. Br J Obstet Gynaecol. 1995;102(1):68-69.
doi pubmed - Lewis DD, Vidovich RR. Organ recovery following childbirth by a brain-dead mother: a case report. J Transpl Coord. 1997;7(3):103-105.
pubmed - Spike J. Brain death, pregnancy, and posthumous motherhood. J Clin Ethics. 1999;10(1):57-65.
pubmed - Vives A, Carmona F, Zabala E, Fernandez C, Cararach V, Iglesias X. Maternal brain death during pregnancy. Int J Gynaecol Obstet. 1996;52(1):67-69.
doi - Wuermeling HB. Brain-death and pregnancy. Forensic Sci Int. 1994;69(3):243-245.
doi - Loewy EH. The pregnant brain dead and the fetus: must we always try to wrest life from death? Am J Obstet Gynecol. 1987;157(5):1097-1101.
doi - Veatch RM. Maternal brain death: an ethicist's thoughts. JAMA. 1982;248(9):1102-1103.
doi pubmed - Milliez J, Cayol V. Palliative care with pregnant women. Best Pract Res Clin Obstet Gynaecol. 2001;15(2):323-331.
doi pubmed - Clark SL, Cotton DB, Lee W, Bishop C, Hill T, Southwick J, Pivarnik J, et al. Central hemodynamic assessment of normal term pregnancy. Am J Obstet Gynecol. 1989;161(6 Pt 1):1439-1442.
doi - Fujitani S, Baldisseri MR. Hemodynamic assessment in a pregnant and peripartum patient. Crit Care Med. 2005;33(10 Suppl):S354-361.
doi pubmed - American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112(24 Suppl):IV1-203.
pubmed - Ogburn PL, Jr., Schmidt G, Linman J, Cefalo RC. Paroxysmal tachycardia and cardioversion during pregnancy. J Reprod Med. 1982;27(6):359-362.
pubmed - Powner DJ, Bernstein IM. Extended somatic support for pregnant women after brain death. Crit Care Med. 2003;31(4):1241-1249.
doi pubmed - Mallampalli A, Guy E. Cardiac arrest in pregnancy and somatic support after brain death. Crit Care Med. 2005;33(10 Suppl):S325-331.
doi pubmed - MM. Maternal cardiovascular, respiratory, and renal adaptation to pregnancy: Elsevier; 2009.
- Crapo RO, Jensen RL, Hegewald M, Tashkin DP. Arterial blood gas reference values for sea level and an altitude of 1,400 meters. Am J Respir Crit Care Med. 1999;160(5 Pt 1):1525-1531.
doi pubmed - Levinson G, Shnider SM, DeLorimier AA, Steffenson JL. Effects of maternal hyperventilation on uterine blood flow and fetal oxygenation and acid-base status. Anesthesiology. 1974;40(4):340-347.
doi pubmed - Brown RW, Diaz R, Robson AC, Kotelevtsev YV, Mullins JJ, Kaufman MH, Seckl JR. The ontogeny of 11 beta-hydroxysteroid dehydrogenase type 2 and mineralocorticoid receptor gene expression reveal intricate control of glucocorticoid action in development. Endocrinology. 1996;137(2):794-797.
doi pubmed - Edwards CR, Benediktsson R, Lindsay RS, Seckl JR. Dysfunction of placental glucocorticoid barrier: link between fetal environment and adult hypertension? Lancet. 1993;341(8841):355-357.
doi - Mercado AB, Wilson RC, Cheng KC, Wei JQ, New MI. Prenatal treatment and diagnosis of congenital adrenal hyperplasia owing to steroid 21-hydroxylase deficiency. J Clin Endocrinol Metab. 1995;80(7):2014-2020.
doi pubmed - Nyirenda MJ, Lindsay RS, Kenyon CJ, Burchell A, Seckl JR. Glucocorticoid exposure in late gestation permanently programs rat hepatic phosphoenolpyruvate carboxykinase and glucocorticoid receptor expression and causes glucose intolerance in adult offspring. J Clin Invest. 1998;101(10):2174-2181.
doi pubmed - de Vries A, Holmes MC, Heijnis A, Seier JV, Heerden J, Louw J, Wolfe-Coote S, et al. Prenatal dexamethasone exposure induces changes in nonhuman primate offspring cardiometabolic and hypothalamic-pituitary-adrenal axis function. J Clin Invest. 2007;117(4):1058-1067.
doi pubmed - Harris A, Seckl J. Glucocorticoids, prenatal stress and the programming of disease. Horm Behav. 2011;59(3):279-289.
doi pubmed - Quinlivan JA, Beazley LD, Archer M, Evans SF, Newnham JP, Dunlop SA. Repeated prenatal corticosteroids reduce glial fibrillary acidic protein in the ovine central nervous system. J Perinat Med. 2002;30(3):209-219.
doi pubmed - Samarasinghe RA, Di Maio R, Volonte D, Galbiati F, Lewis M, Romero G, DeFranco DB. Nongenomic glucocorticoid receptor action regulates gap junction intercellular communication and neural progenitor cell proliferation. Proc Natl Acad Sci U S A. 2011;108(40):16657-16662.
doi pubmed - In: Rasmussen KM, Yaktine AL, editors. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC); 2009.
- Nuutinen LS, Alahuhta SM, Heikkinen JE. Nutrition during ten-week life support with successful fetal outcome in a case with fatal maternal brain damage. JPEN J Parenter Enteral Nutr. 1989;13(4):432-435.
doi pubmed - Gandra S, Ellison RT, 3rd. Modern Trends in Infection Control Practices in Intensive Care Units. Journal of intensive care medicine. 2013. Epub 2013/06/12.
- Edwards MJ. Hyperthermia as a teratogen: a review of experimental studies and their clinical significance. Teratog Carcinog Mutagen. 1986;6(6):563-582.
doi pubmed - Gluckman PD, Gunn TR, Johnston BM. The effect of cooling on breathing and shivering in unanaesthetized fetal lambs in utero. J Physiol. 1983;343:495-506.
pubmed - Gherman RB, Goodwin TM, Leung B, Byrne JD, Hethumumi R, Montoro M. Incidence, clinical characteristics, and timing of objectively diagnosed venous thromboembolism during pregnancy. Obstet Gynecol. 1999;94(5 Pt 1):730-734.
doi - Toglia MR, Weg JG. Venous thromboembolism during pregnancy. N Engl J Med. 1996;335(2):108-114.
doi pubmed - Prevention of venous thrombosis and pulmonary embolism. NIH Consensus Development. JAMA. 1986;256(6):744-749.
doi pubmed - Bremme KA. Haemostatic changes in pregnancy. Best Pract Res Clin Haematol. 2003;16(2):153-168.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.